Inmates with Dementia: The Unseen Impact of Aging Behind Bars
In 2024, the last of the Baby Boomers, including myself, will turn 60. As the American population of baby boomers becomes geriatric, we also have an aging population in our prisons. 15% of American prisoners are above 55 and 32% of those elderly prisoners are black men. They may have life sentences or have been caught up in “tough against crime” terms. And some of them are becoming mentally ill in environments not trained to deal with them.
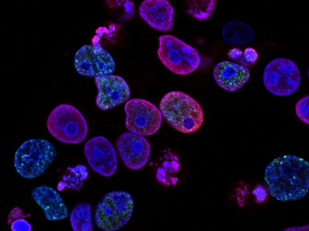
Psychologists, researchers, aging councils and Alzheimer’s institutions have been looking at this problem for the last 20 years, as the population of inmates with dementia may reach 20,000 by 2030. There has been progress, but not enough to prepare for the surging population of elderly inmates.
Here in the outside world, we know that dementia patients need structure, understanding, patience, and sometimes 24-hour care. We know that their memories are impaired, sometimes forgetting their loved ones, or not remembering that someone has died. We know that they may not be able to cook, clean, drive. Worse still, they may not remember when and where to urinate. Tragically, some advanced dementia patients, dealing with fear and paranoia, turn violent, hurting loved ones and professional caregivers alike. They can be hard to control or direct, stubborn and unyielding. They wander, they get lost. For all of these reasons, we have created special places for our demented elderly when families are not in a position to take care of them.
And that is what happens in the outside world. The prison environment is vastly different. It houses criminals who may have lower intelligence, may be substance abusers, are in poorer health and in general may be more physiologically disposed to dementia. It is said that the incarcerated age 15 years faster than those in the outside world, because of the stress caused by living in prison, from depression to lack of stimulation to assault. So, by age 50, prisoners are exhibiting the chronic illnesses associated with the elderly – from diabetes to arthritis to strokes… to dementia.
You might think that the humane thing to do is to let them go. Decarcerate them, commute their sentences: compassionate release. In 1989, a program was developed for just that purpose. POPS – the Project for Older Prisoners. It was intended to address prison overcrowding by identifying prisoners with a low risk of recidivism, grooming them for the outside world, and doing the legal work to get them an early release. The Federal Bureau of Prisons initiated a similar program of compassionate release for patients with severe medical problems or dementia who are over 60 and have served over half of their sentences. But recent data indicates that the structure of these programs and their eligibility requirements have resulted in very few inmates being released. Moreover, this might not be the solution for violent offenders who are too old to work, have nowhere to go, no money for private care, and a criminal record that excludes them from most nursing homes. Society is not prepared to have violent offenders in the same space as their loved ones.
Instead, many state prisons are trying an alternative – setting aside an environment for the demented where they are cared for while they are in prison, sometimes by licensed caregivers and sometimes by their incarcerated peers. It may be surprising that states are choosing to do this, but many have weighed the costs. Providing in-prison care is cheaper than paying the Medicaid costs of placing someone in private care. In 2012 in California for example, there are “Gold Coats”, incarcerated men, often violent killers, who are choosing to get the training to care for dementia patients in return for pay and the possibility of early parole. It is amazing how well the program is working. In New York, Pennsylvania, and Illinois, there are special units for those requiring dementia care with an interdisciplinary staff. Louisiana has a system similar to California’s. The first federal prison to try a special setting for geriatric prisoners with dementia was in Massachusetts in 2019 with the 36-bed Memory Disorder Unit, with trained inmate CNAs.
Sadly, these efforts may not be enough to take care of the anticipated population. More states need to prepare, more federal medical centers (prisons) need to prepare. One possibility is to ramp up POPS programs, and drastically increase the number of inmates who are compassionately released, especially those that have family who can care for them. Alternatively, state prisons need to increase their elder care facilities. It won’t be a popular topic – prison issues rarely are – but prisons will need more money, and as a society, we need to care for everyone. Including those in prison.







Comment (1)
You have mentioned very interesting points! ps decent website.Raise your business